As with the surgical procedure for female sterilisation, known as tubal ligation, the vasectomy is an operation that aims to be definitive, and which results in a man not being able to have children naturally, and will therefore be sterile. For this reason, it is important to be very aware of the decision and to weigh up the pros, as well as the cons, of undergoing it.
Vasectomy is a very effective method of contraception, which is difficult to reverse. It can only be done through another, more extensive, surgical process. Men who take this decision are either very sure that they do not want to experience fatherhood, or they do not want to have any more children, and in most cases, it is a decision made jointly with their partner.
We at Eugin understand this and we also know how important it is to be able to help you fulfil your desire to become parents in the future, whether it is for the first time or not.
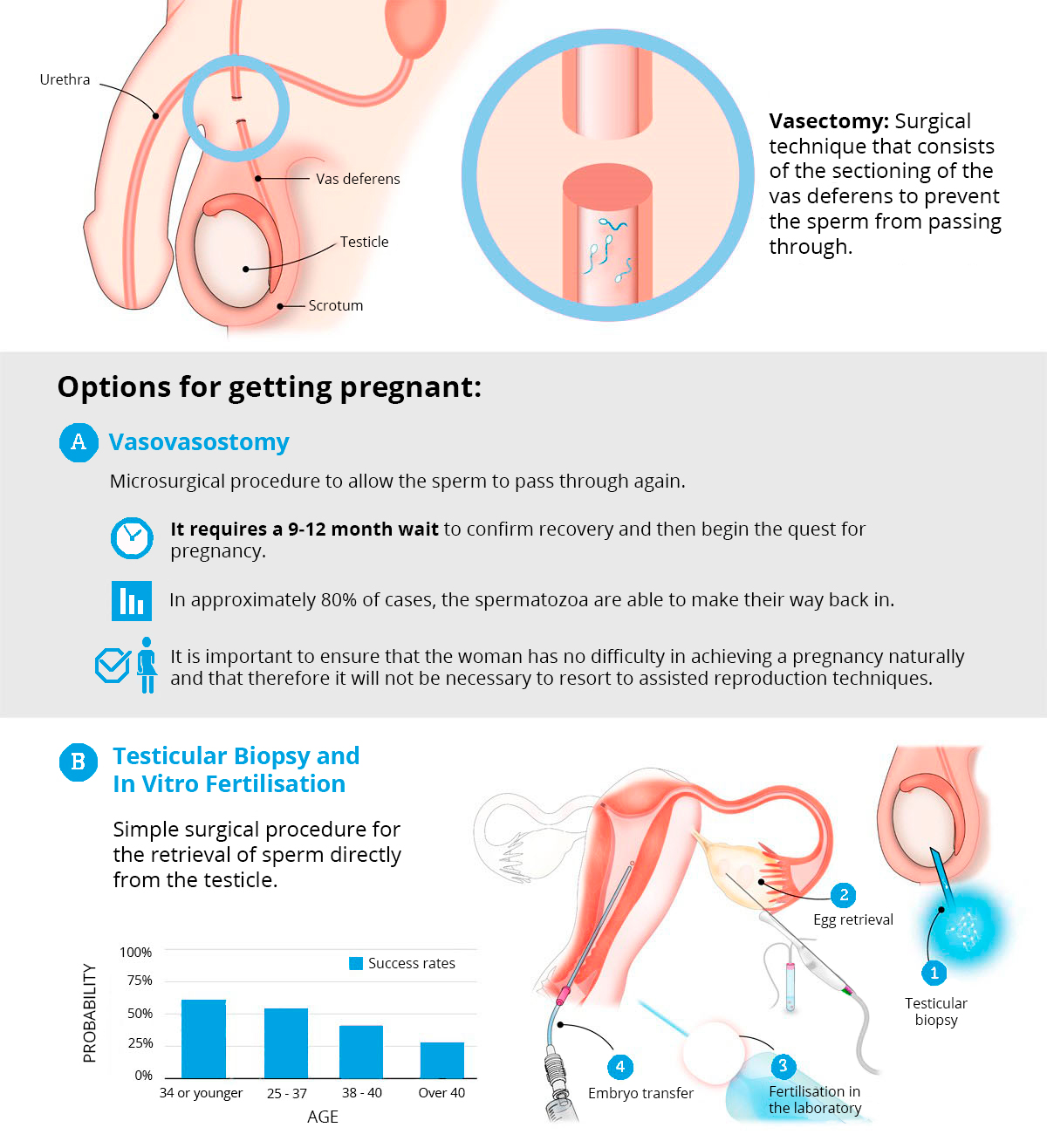
What in the past was considered a method of permanent sterilisation, can now be reversed thanks to medical and technological innovations, and it makes it possible for a man to become fertile again, by means of even more invasive surgery, although this is an operation that does not always achieve its objective and requires a waiting period after it has been carried out. In addition, there are other options to consider if a man wants to be a father, but does not want to go through an operation again, such as, for example, in vitro fertilisation involving a testicular biopsy.
This latter option is the most common in couples who find themselves in this type of situation, and want to become parents, because in this way, they can try to conceive with greater chances of success.
Can you be a father after a vasectomy? What are the options? We will see below the drawbacks and complications that may occur during the process.
Vasectomy is the most established, definitive and reliable male contraceptive procedure.
This is surgery to cut the vas deferens, which are the tubes that allow sperm to pass from the testicles to the urethra. After this operation, the sperm cannot move out of the testes and cannot be expelled with the ejaculation, so the man will not be able to make a woman pregnant.
A vasectomy is usually performed under local anaesthetic and involves making a small incision in the upper part of the scrotum so that the vas deferens can be ligated and cut. The small wound is closed with stitches.
It is important to note that, after the operation, there will still be some sperm circulating in the seminal fluid, i.e. sterilisation will not be complete until they are cleared or die, so the weeks (up to 3-6 months) following the vasectomy will still require the use of other contraceptive methods. Usually a follow-up seminogram is performed after a few weeks to certify the effectiveness of the method.
Some interesting facts about this male sterilisation process are:
- It is important to note that this contraceptive method does not protect against the transmission of sexually transmitted diseases (STDs).
- It does not affect a man’s sexual function, he can have sex as soon as he feels ready and there will be no difference compared to prior to the operation.
- A vasectomy does not increase the risk of diseases such as prostate cancer or testicular disease.
Infertility in men who have had family planning surgery (vasectomy) is a fairly frequent problem as everyone’s circumstances can change, leading to a reconsideration of situations previously thought irreversible. Human Reproduction is a specialised area of medicine which shares the knowledge of reproductive Gynaecology and Biology. It has developed techniques to identify and treat sometimes complex sterility cases, and has enough resources to help patients who want to have a child after having undergone a vasectomy.
The current therapeutic procedures are:
- In Vitro Fertilisation (IVF) with intracytoplasmic sperm injection (ICSI); sperm is retrieved from a testicle, epididymis or deferent duct.
- Microsurgical repair of the seminal duct (vasovasostomy).
The factors that determine the choice of the therapeutic procedure are first of all the woman’s age (older or younger than 35), and the likelihood of more than one pregnancy in the future.
In the case where the woman is older than 35, and/or the couple do not want to have another child once they have had the first one, the recommended treatment is surgical sperm retrieval in conjunction with IVF-ICSI.
With this alternative the time between carrying out the treatment and the possible resulting pregnancy is quite short and, when no other pregnancy is desired, it is not necessary for the couple to take contraceptive precautions.
If repermeability of the sperm ducts is required in order to bring about a spontaneous pregnancy, then the appropriate treatment is a microsurgical repair of the deferent ducts. When the outcome of the operation is satisfactory and there are spermatozoa when ejaculation occurs and a spontaneous gestation occurs, the couple must take contraceptive precautions if they do not wish have more children.
Moreover, with this technique the time needed to see the results is longer and, therefore, it is not advised for women older than 35.
In the case when after a vasovasostomy a pregnancy does not occur due to the absence, or insufficient quantity of spermatozoa or a lack of them, Assisted Reproduction Techniques (FIV-ICSI) can be considered.
This is made up of a series of tests and analyses which are carried out in order to investigate the theoretical fertility of the couple before considering an IVF-ICSI cycle:
For women
- A blood test is carried out to check that there are no hormonal alterations (FSH, LH and Estradiol).
- A hysteroscopy may be done if there is a chance of an existing pathology. This is a cervix exploration which is carried out without the need of anaesthesia. It allows us to diagnose certain problems and suggest treatments to help solve them. For example, if a myoma or a polyp is identified, the course of treatment would be their removal. This can be carried out during the actual procedure, or could be scheduled for the future.
For men
For men, a testicular biopsy is carried out under local anaesthetic to obtain the spermatozoids (a sample of the testicular tissue is removed). This proceedure can be carried out on the same day as the IVF-ICSI treatment or at the start of the IVF-ICSI cycle. If it were to be the latter, the sample would be frozen and then thawed on the day of the IVF-ICSI.
In general, when the woman does not have a sterility problem, a semen sample of sufficient quality (to retrieve enough spermatozoa) has to be obtained to fertilise the eggs.
Assisted Reproduction Treatments are a series of delicate techniques carried out jointly by Gynaecologists, Andrologists and Biologists in specialised centres.
- Testicular biopsy
- Reconstructive microsurgery of the seminal duct (vasovasostomy)
1.- Testicular biopsy
It is carried out under local anaesthetic and consists of removing a sample of the testicular tissue. This sample is studied under a microscope, and the spermatozoids are identified and saved. These will be used to fertilise the woman’s eggs, or frozen and kept for the same purpose. Unless the Intracytoplasmic sperm injection (ICSI) is carried out, the quantity of spermatozoids obtained from the testicular biopsy are insufficient to go ahead with an In Vitro procedure.
2.- MVasovasostomy:
A vasovasostomy is a precise surgical procedure which aims to rejoin the deferent duct incised during the vasectomy. The vasovasostomy is carried out under local anaesthetic. The surgical magnifying glass is used as the spermiduct has to be restored joining both ends. First new tissue is created by removing the scarred proximal and distal ends (the ends where the deferent was cut) and then they are brought together and stitched with a very fine thread.
Once the vasovasostomy has been performed, several months have to pass for the results to be seen (for enough spermatozoa to be present when ejaculation occurs). Although a vasovasostomy appears to be a simple solution for a vasectomy, in reality this technique is somewhat complex.
Though not usual, sometimes it is impossible to carry out the vasovasostomy correctly as the ends of the deferent duct can break away or fail to join.
Even when the surgery is successful, the result is not always guaranteed as it is not enough to just join both ends of the deferent duct together. Its ability to transport the seminal liquid has to be recovered but the outcome of the procedure is not known at the moment of the surgery. Spermatozoa may not be present.
Although the two previous difficulties may be successfully overcome, the amount of sperm might not be sufficient to carry out Artificial Insemination. Therefore, IVF-ICSI treatment has to be considered as in the above case.
Nowadays it is more advisable to proceed with IVF-ICSI when a couple wants a child after having a vasectomy. On the other hand, when a couple wants to start a new family and have several children a vasovasostomy can be a practical alternative, especially when the woman is young enough to remain fertile for some years.
Even though at the time of undergoing it you have to be 100% sure of the decision in order to avoid risks, vasectomy is a contraceptive method that not only offers great advantages for men, but does so for women too. It is a method that, in addition to its high reliability, avoids the risks that other contraceptive methods entail for women. An example of this is the adverse effects of oral contraceptives or tubal ligation surgery, which involves more extensive surgery and may entail greater risks and a slower and more painful post-operative process. In addition, vasectomy has no effect on male sexual function. In fact, you may enjoy sex more, since there is no longer any concern about an unwanted pregnancy.
If you need more information about the possibility of becoming a father after a vasectomy, we at Eugin will be happy to help both you and your partner, with the possibility of conceiving through in vitro fertilisation, thus avoiding having to go through more invasive surgical procedures.
Do you have a query that can’t wait? Ask our experts.
